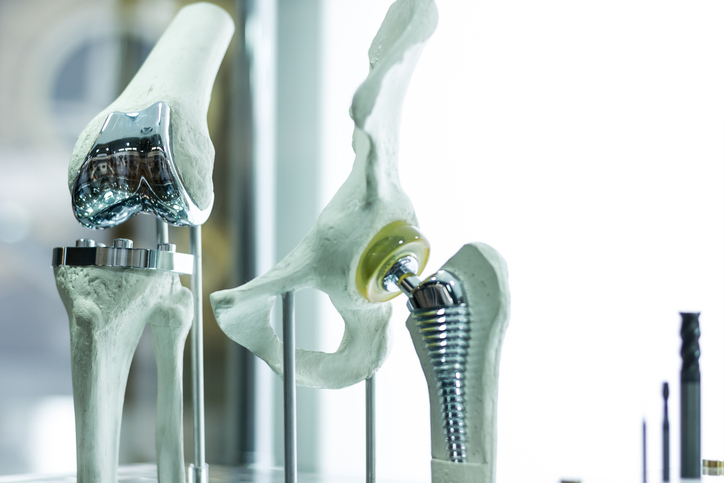
 The development of prosthetics has changed many lives, providing mobility options and allowing for more active lives. But all artificial limbs aren’t perfect. Some can be painful, difficult to use, and lead to possible skin infections. The Office of Naval Research is looking to change that, providing new options for those in need of artificial limbs.
The development of prosthetics has changed many lives, providing mobility options and allowing for more active lives. But all artificial limbs aren’t perfect. Some can be painful, difficult to use, and lead to possible skin infections. The Office of Naval Research is looking to change that, providing new options for those in need of artificial limbs.
By teaming up with the Walter Reed National Military Medical Center, the Office of Naval Research has developed a “smart” artificial leg, using sensor technology to monitor walking, alter the way the user wears the prosthetic to aid in comfortability and reduce wear and tear, and warn of potential infection risks. They’re referring to this development as Monitoring Ossolntegrated Prosthesis (MOIP).
“This new class of intelligent prostheses could potentially have a profound impact on warfighters with limb loss,” says Liming Salvino, a program officer in ONR’s Warfighter Performance Department. “MOIP not only can improve quality of life, but also usher in the next generation of prosthetic limbs.”
This from the Office of Naval Research:
The advantages of osseointegrated prosthetics include less pain, a fluid walking motion and a more stable, better-fitting limb. But because metal sticks out of the residual limb, infection is a constant risk. To address this issue, MOIP will focus on infection detection, eradication and prevention—by developing both electrochemical sense-and-respond approaches and “smart” skin technologies.
The sensory array in this technology is the first of its kind. It tracks body temperature and pH balance, which can indicate possible infection. It can also examine how well the bone and prosthetic limb are working together.
“One game-changing application of this technology would be as a tool to inform doctors when prosthetics can be safely loaded after surgery, leading to more accurate determination of when patients are ready for physical therapy after receiving a new prosthetic,” says Jerome Lynch, a University of Michigan engineering professor who is overseeing the sensor array’s development. “Right now, doctors study X-ray images of a limb when making that determination. Because the sensors transmit information wirelessly, doctors also could potentially study patient data via a handheld reader. Think of it as an extremely specialized Fitbit. This could dramatically improve the recovery and long-term quality of life for patients.”