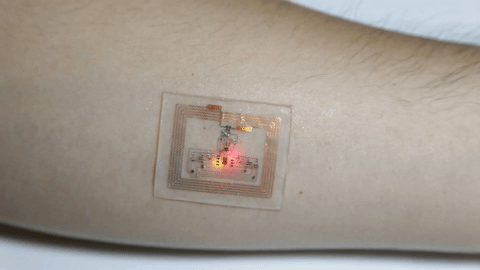
Researchers at Northwestern University and Washington University School of Medicine have developed the first example of a bioelectronic medicine, according to ScienceDaily. The biodegradable, implantable, wireless device was created with the goal to speed up nerve regeneration in nerve injury patients. It works by delivering pulses of electricity to damaged nerves, accelerating regrowth, and also enhancing the recovery of muscle strength and control.
Not only does the new technology improve healing time, there’s also no need to worry about undergoing a separate procedure for removal. The implant, about the size of a dime and the thickness of a sheet of paper, absorbs naturally into the body about a week or two after implantation, taking care of its own disposal. (more…)




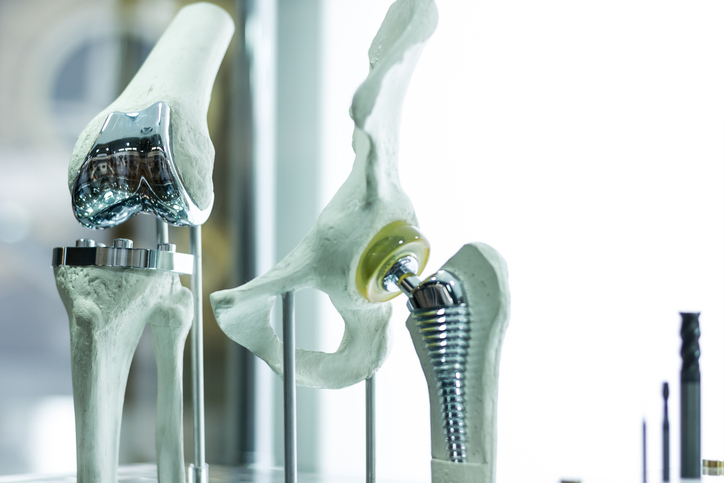 The development of prosthetics has changed many lives, providing mobility options and allowing for more active lives. But all artificial limbs aren’t perfect. Some can be painful, difficult to use, and lead to possible skin infections. The Office of Naval Research is looking to change that, providing new options for those in need of artificial limbs.
The development of prosthetics has changed many lives, providing mobility options and allowing for more active lives. But all artificial limbs aren’t perfect. Some can be painful, difficult to use, and lead to possible skin infections. The Office of Naval Research is looking to change that, providing new options for those in need of artificial limbs.